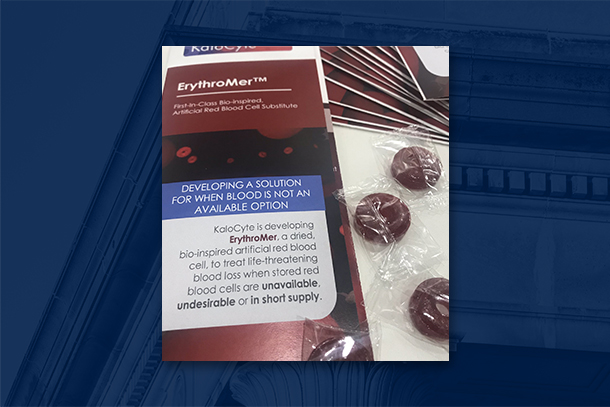
Penn State Professor Dipanjan Pan co-invented ErythroMer, an artificial oxygen carrier, that will be used in a $46 million project led by the University of Maryland School of Medicine to develop an artificial whole blood product. Credit: Provided by Dipanjan Pan/Penn State. All Rights Reserved.
Penn State scientist plays key role in $46M artificial blood research program
Dipanjan Pan co-invented a blood product to be used in DARPA project
March 27, 2023
Editor's note: A version of this story first appeared on the University of Maryland Baltimore’s website.
UNIVERSITY PARK, Pa. — The Defense Advanced Research Projects Agency (DARPA) is administering a $46.4 million, four-year research project to develop and test a whole blood product that is storable at room temperature and can be transfused to wounded soldiers in the field within 30 minutes of injury.
Dipanjan Pan, Dorothy Foehr Huck & J. Lloyd Huck Chair Professor in Nanomedicine and professor of nuclear engineering and of materials science and engineering at Penn State, will serve as a co-investigator on the project. Pan is also affiliated with the Penn State Department of Biomedical Engineering.
The University of Maryland School of Medicine (UMSOM) will manage the project in collaboration with the University of Maryland School of Pharmacy and more than a dozen universities and biotech companies, including Penn State. Pan will lead the consortium’s nano and bioengineering domain.
Pan co-invented ErythroMer, the artificial blood product that the project will use. The ErythroMer technology was licensed by KaloCyte, a company co-founded by Pan; project principal investigator Allan Doctor, professor of pediatrics and director of the Center for Blood Oxygen Transport and Hemostasis at UMSOM; and Philip Spinella, a military transfusion medicine expert at the University of Pittsburgh.
“The synthetic blood project began many years ago in our labs, then at Washington University in St. Louis,” Pan said. “Through a serendipitous discovery, we developed uniquely shaped particles that mimic red blood cells and found that they could carry very high payload of hemoglobin. Through extensive biological characterization and animal studies with Doctor’s lab, we identified that these particles could deliver oxygen to trauma patients. The pursuit to create artificial blood in laboratory isn’t new; however, all previous attempts failed. We approached this problem very differently and our strategy addressed all the design flaws from prior failed attempts. So, it will be the first successful attempt at developing a context-responsive oxygen carrier in the lab.”
Pan’s academic team, in collaboration with Doctor, previously received funding for this project from the Department of Defense, the National Institutes of Health and other organizations.
The DARPA-administered consortium will use a more refined, second generation of this blood product that can carry oxygen, in conjunction with synthetic platelets and freeze-dried plasma to develop a “whole blood product,” according to Pan.
“We have assembled an outstanding team to develop a bio-synthetic whole-blood product that can be freeze-dried for easy portability, storage and reconstitution,” Doctor said. “It will be designed for easy use in the field by medics at the point of injury and will perform like a traditional blood transfusion to, for example, stabilize a patient’s blood pressure or facilitate blood clotting.”
According to Pan, the first phase of the study will involve integrating multiple bio-artificial and synthetic components to facilitate key therapeutic functions of whole blood in resuscitation: deliver oxygen, stop bleeding and replace volume. In the second phase, the team will evaluate efficacy and safety in increasingly complex and realistic trauma models, Pan said. This phase will also involve developing strategies for stabilizing the product for months under ambient climate conditions in extreme environments.