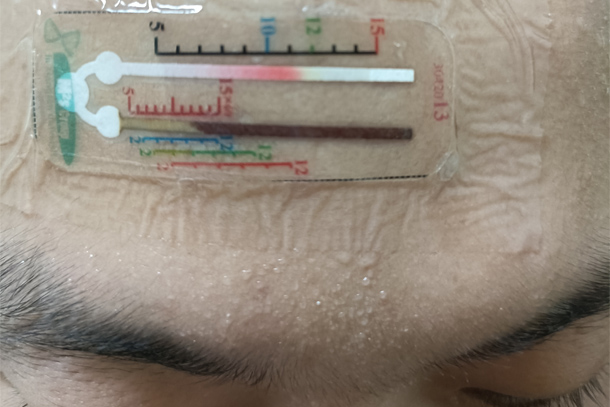
A wearable sensor, developed by Penn State researchers, accurately detects biomarker concentrations in sweat samples. Credit: Provided by Larry Cheng
Two-channel sensor measures biomarker concentration in sweat
The novel easy-to-use device has implications for diagnostic testing, especially in remote areas
January 4, 2024
By Sarah Small
UNIVERSITY PARK, Pa. — Sensors applied to the skin hold promise for a non-invasive and low-cost method of identifying key biomarkers in sweat, which could help clinicians make earlier and more accurate diagnoses. Up until now, however, sensors could identify the presence of biomarkers but lacked the ability to accurately detect their concentration in the presence of erratic, intermittent and unpredictable sweat production.
To solve this problem, a team of Penn State researchers has developed a sensor that accurately detects biomarker concentrations in sweat samples. Their work was published in Advanced Science.
While researchers had previously created a sensor that could detect amounts of glucose and other biomarkers, the sensors lacked a way to accurately detect the volume of sweat, meaning the concentration of the biomarkers was unknown.
“One particular challenge is to quantify that biomarker and sweat rate in an accurate manner, because the different conditions that cause us to sweat — exercise, warm weather, eating spicy foods — can all have different rates of sweating that may be more consistent or may be on-and-off sweating,” said Huanyu “Larry” Cheng, the James L. Henderson, Jr. Memorial Associate Professor of Engineering Science and Mechanics at Penn State. “That makes it challenging to measure the volume of sweat, which we need to know if we want to quantify the biomarker concentration.”
To assess this information, the researchers designed a sensor with two channels for capturing sweat: one that will measure the amount of the biomarker, and one that will measure the volume of sweat. The sensor relies on a dye to signal the presence of the biomarker and can be read with the naked eye, making it inexpensive and easy to use. According to Cheng, because the sensor’s results can be so easily read without expensive processing equipment, it could be especially useful to providers in remote areas.
“The liquid will react with the dye deposited in the channel, changing color, and based on the advancing front of the liquid, we can quantify the sweat rate and volume based on the line in that channel,” Cheng said. “We use the printed marks near the channel to indicate the sweat volume to compare with, and then use the other set of marks to read out the concentration at the pre-set volumes.”
The concentration of the biomarker, not just its presence, is useful in diagnostics. For example, the researchers said their sensor could be used to test for cystic fibrosis, which is often indicated by high levels of chloride in the patient.
“The typical course of action to diagnose cystic fibrosis is to induce a local sweat through exercise, but with our sensor, we can detect the chloride concentration in sweat without requiring the patient to exercise, since we can use passive heat-induced sweating with our wearable form of the testing setup,” Cheng said.
This method, combined with the soft materials of the sensor, makes it better than traditional diagnostic testing for infants and young children, according to Cheng. To test the sensor, Cheng is partnering with doctors at the Milton S. Hershey Medical Center for a trial of the sensor.
Muhan Deng, Xiaofeng Li, Hanglin Yang, Wenkui Wei, Xiaoping Ouyang and Xiufeng Wang, all of Xiangtan University in China, were co-authors on the paper. This work was supported in part by the National Science Foundation, the National Institutes of Health, the National Natural Science Foundation of China and the Natural Science Foundation of Hunan Province.