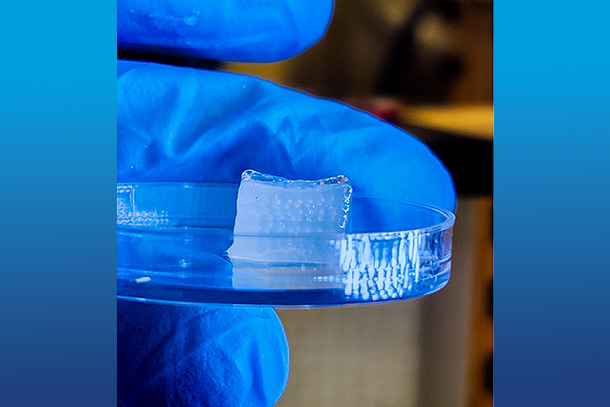
Researchers printed a centimeter cube cartilage construct via high-throughput Integrated Tissue Fabrication System for Bioprinting (HITS-Bio). Credit: Courtesy of Ozbolat Lab at Penn State / Penn State.
New bioprinting technique creates functional tissue 10x faster
The novel high-throughput-bioprinting technique opens the door for tissue fabrication with high cell density at scale
Dec 3, 2024
Editor's note: This article originally appeared on Penn State News.
By Christine Yu
UNIVERSITY PARK, Pa. — Three-dimensional (3D) printing isn’t just a way to produce material products quickly. It also offers researchers a way to develop replicas of human tissue that could be used to improve human health, such as building organs for transplantation, studying disease progression and screening new drugs. While researchers have made progress over the years, the field has been hampered by limited existing technologies unable to print tissues with high cell density at scale.
A team of researchers from Penn State have developed a novel bioprinting technique that uses spheroids, which are clusters of cells, to create complex tissue. This new technique improves the precision and scalability of tissue fabrication, producing tissue 10-times faster than existing methods. It further opens the door to developing functional tissues and organs and progress in the field of regenerative medicine, the researchers said.
They published their findings in Nature Communications.
“This technique is a significant advancement in rapid bioprinting of spheroids,” said corresponding author Ibrahim T. Ozbolat, Dorothy Foehr Huck and J. Lloyd Huck Chair in 3D Bioprinting and Regenerative Medicine and professor of engineering science and mechanics, of biomedical engineering and of neurosurgery at Penn State. “It enables the bioprinting of tissues in a high-throughput manner at a speed much faster than existing techniques with high cell viability.”
Bioprinting allows researchers to build 3D structures from living cells and other biomaterials. Living cells are encapsulated in a substrate like a hydrogel to make a bioink, which is then printed in layers using a specialized printer. These cells grow and proliferate, eventually maturing into 3D tissue over the course of several weeks. Ozbolat explained that it’s like constructing a brick wall where the cells are the bricks and the bioink is the cement or mortar.
However, it’s difficult to achieve the same cell density as what’s found in the human body with this standard approach, Ozbolat said. That cell density is essential for developing tissue that’s both functional and can be used in a clinical setting. Spheroids, on the other hand, offer a promising alternative for tissue bioprinting because they have a cell density similar to human tissue.
While 3D printing spheroids offers a viable solution to producing the necessary density, researchers have been limited by the lack of scalable techniques. Existing bioprinting methods often damage the delicate cellular structures during the printing process, killing some of the cells. Other technologies are cumbersome and don’t offer precise control of the movement and placement of the spheroids needed to create replicas of human tissue.
Or the processes are slow. In previously published research, Ozbolat and his colleagues developed an aspiration-assisted bioprinting system. Using a pipette tip, the researchers could pick up tiny balls of cells and place them precisely where they self-assemble and create a solid tissue. However, since the technique involves moving spheroids one at a time, it could take days to build a one cubic centimeter structure.
To address these issues, the team developed a new technique called High-throughput Integrated Tissue Fabrication System for Bioprinting (HITS-Bio). HITS-Bio uses a digitally controlled nozzle array, an arrangement of multiple nozzles that moves in three dimensions and allows researchers to manipulate several spheroids at the same time. The team organized the nozzles in a four-by-four array, which can pick up 16 spheroids simultaneously and place them on a bioink substrate quickly and precisely. The nozzle array can also pick up spheroids in customized patterns, which can then be repeated to create the architecture found in complex tissue.
“We can then build scalable structures very fast,” Ozbolat said. “It’s 10-times faster than existing techniques and maintains more than 90% high cell viability.”
To test the platform, the team set out to fabricate cartilage tissue. They created a one-cubic centimeter structure, containing approximately 600 spheroids made of cells capable of forming cartilage. The process took less than 40 minutes, a highly efficient rate that surpasses the capacity of existing bioprinting technologies.
The team then showed that the bioprinting technique can be used for on-demand tissue repair in a surgical setting in a rat model. They printed spheroids directly into a wound site in the skull during surgery, which was the first time spheroids have been printed intraoperatively. The researchers programmed the spheroids to transform into bone using microRNA technology. MicroRNA helps control gene expression in cells, including how cells differentiate into specific types.
“Since we delivered the cells in high dosages with this technique, it actually sped up the bone repair,” Ozbolat said. The wound was 91% healed after three weeks and 96% healed after just six weeks.
The HITS-Bio technique offers an opportunity to create complex and functional tissue in a scalable manner, Ozbolat said. Expanding the number of nozzles could lead to production of larger and more intricate tissues, such as organs and organ tissue like the liver.
Ozbolat said that the team is also working on techniques to incorporate blood vessels into the fabricated tissue, a necessary step for producing more types of tissues that can be used clinically or for transplantation. This wasn’t an issue with the two applications demonstrated in this study because cartilage has no blood vessels and, in a surgical setting, the surrounding blood vessels could help with blood flow to the bioprinted bone tissue.
Other Penn State authors include: Myoung Hwan Kim, doctoral student in biomedical engineering; Yogendra Pratap Singh and Miji Yeo, postdoctoral scholars in engineering science and mechanics; Daniel Hayes, Dorothy Foehr Huck and J. Lloyd Huck Chair in Nanotherapeutics and Regenerative Medicine; and Elias Rizk, professor of neurosurgery at the Penn State College of Medicine. Co-author Nazmiye Celik was a doctoral scholar in engineering science and mechanics at the time of the study and is now a postdoctoral fellow at Johns Hopkins University.
Ozbolat, Kim, Singh, Yeo and Hayes are affiliated with the Huck Institutes of the Life Sciences. Ozbolat and Hayes are also affiliated with the Penn State Materials Research Institute. Ozbolat is also affiliated with the Penn State Cancer Institute.
Funding from the National institute of Biomedical Imaging and Bioengineering and the National Institute of Dental and Craniofacial Research supported this work.