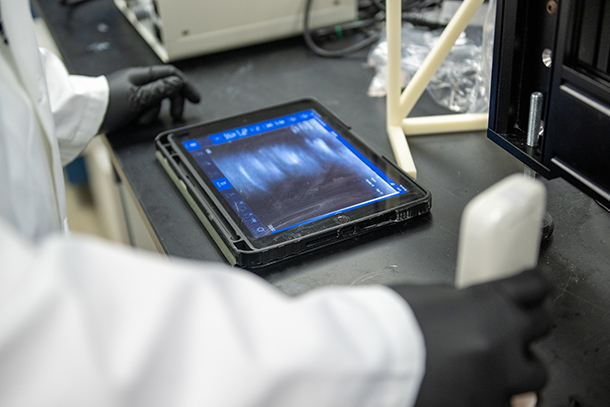
With a four-year, $2,276,850 National Institutes of Health grant, Penn State researchers aim to create a completely non-invasive, tunable method for treating tendinopathies with focused ultrasound. Credit: Jeff Xu/Penn State. All Rights Reserved.
Engineers awarded NIH grant to heal tendon injuries with ultrasound
March 8, 2023
By Sarah Small
UNIVERSITY PARK, Pa. — Tendon pain or injuries, known as tendinopathies, impact everyone from athletes to manual laborers to others performing daily activities. A controllable, noninvasive method of treatment has remained elusive, but with a four-year, $2,276,850 National Institutes of Health grant, Penn State researchers are planning to change that. The researchers, led by Julianna Simon, Penn State assistant professor of acoustics and of biomedical engineering, aim to create a completely non-invasive, tunable method for treating tendinopathies with focused ultrasound.
According to Simon, the project has two main components.
“First, we're trying to prove that we can use ultrasound to basically create a hole in a tendon,” she said. “We're also developing a treatment where, instead of a hole, we use just a little bit of bubble activity to create these micropores. They allow healing factors in and waste out.”
The “bubble activity” refers to the creation of voids with ultrasound, Simon explained. Sound is a pressure wave that compresses and pulls apart repeatedly. Ultrasound is any sound above 20,000 oscillations per second or Hertz, which is the upper limit for human hearing. When the energy is focused, it can generate enough energy to pull apart the tissue to create the void, or bubble.
“It's going to oscillate, and then, if you push on it hard enough, it's going to actually collapse violently, and that's where you can create some therapeutic effects,” Simon said.
The researchers will test their treatment in animal models to see how such therapeutic effects, including disrupting scar tissue formation, may help the tendons heal better.
“We also hope that we can cause collagen alignments as the tendon heals,” Simon said. “In addition to scar tissue when the tendon heals, you get all these fibers at all sorts of angles. If we can help them align in a more parallel structure, that would help the strength of that healed tendon, so now it can resist a lot more load.”

Julianna Simon, Penn State assistant professor of acoustics and of biomedical engineering, connects a transducer matching network prior to the focused ultrasound treatment. Credit: Jeff Xu/Penn State. All Rights Reserved.
Simon said that these positive therapeutic effects can also be created through heat from the ultrasound.
“All of the ultrasound energy gets absorbed by the tissue and can literally cook the tissue,” she said. “And one of the advantages of focused ultrasound over other modalities is that we can very precisely control where that focus is. We don't damage any of the tissue in the intervening pathway, but we can treat deep in the body and get these effects through either heat or bubble activity.”
Conventional methods of treating tendinopathy, including dry needling, may work on some patients and not on others, Simon said. The problem is that researchers do not yet understand why some of these methods work some of the time on some people. By using the ultrasound imaging, Simon and her team hope to target exactly where the injury is and treat it noninvasively in a controllable manner. The ultimate goal is clinical translation for use in humans, Simon said.
Meghan Vidt, assistant professor of biomedical engineering and of physical medicine and rehabilitation, and Erin Luley, assistant clinical professor in the Department of Veterinary and Biomedical Sciences and veterinary anatomic pathologist, both at Penn State, will also lead components of this research.
The researchers will collaborate with veterinary staff and will follow a protocol approved by Penn State’s Institutional Animal Care and Use Committee.