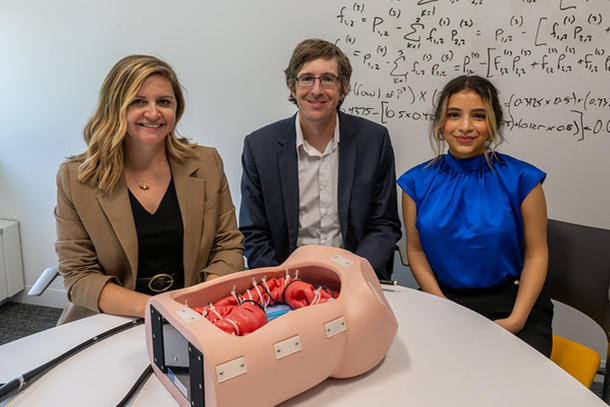
Scarlett Miller, professor of engineering design and industrial engineering and director of the Center for Research in Design and Innovation, Jason Moore, professor of mechanical engineering, and Eric Pauli, professor of surgery at the Penn State College of Medicine, discussed their novel colonoscopy training system with Penn State News in a Q&A. From left to right: Scarlett Miller, Jason Moore, and Isra Elsaadany, doctoral student in industrial engineering. Credit: Kate Myers/Penn State
Q&A: Enhancing physicians’ colonoscopy training for early cancer prevention
Multidisciplinary team awarded $1.7M NIH grant to make the routine procedure safer, more accurate
November 15, 2023
By Tessa M. Pick
UNIVERSITY PARK, Pa. — A novel colonoscopy training system that integrates automated personalized learning with a manikin — the more realistic version of a mannequin capable of medical simulations — embedded with sensors may help make the routine procedure safer, more accurate and cost-efficient. That’s the goal of a team led by Penn State College of Engineering researchers that received a $1.7 million grant from the National Institutes of Health’s National Institute of Diabetes and Digestive and Kidney Diseases to further develop the new system, deploy it and examine its effectiveness.
The research team is led by Scarlett Miller, professor of engineering design and industrial engineering and director of the Center for Research in Design and Innovation, and Jason Moore, professor of mechanical engineering, and also includes Eric Pauli and Randy Haluck, professors of surgery at the Penn State College of Medicine, and Isra Elsaadany, second-year doctoral student in industrial engineering.
The researchers discussed the work with the College of Engineering in the Q&A below:
Q: What is the prevalence of colonoscopy procedures and what is their clinical purpose?
Miller: Colonoscopies provide physicians with minimally invasive access to diagnose and treat diseases such as colorectal cancer — the third-most common and second-most lethal type of malignancy in the U.S. More than 19 million colonoscopies are performed in the U.S. each year, with 60% of adults ages 55 to 75 having at least one within the last decade. Colonoscopies are also one of the most expensive screening tests routinely performed on healthy Americans, with a mean cost of $2,125 per procedure.
Q: Why are advanced simulators needed for colonoscopy training?
Miller: Early detection from preventative screening through colonoscopies can drastically improve outcomes for colorectal cancer. When caught at an early stage, 90% of adults diagnosed with colorectal cancer live for five or more years. However, up to 28% of polyps are missed during screening, leading to a high false-negative cancer detection rate. Lack of appropriate identification can lead to multiple procedures and unnecessary health care costs. When it comes to training, it takes physicians more than 400 patient cases to achieve benchmarks set by the medical profession for locating and identifying polyps throughout the colon. This number far surpasses the 50-case requirement for surgical residency, as required by the Defined Category Minimum Numbers for General Surgery Residents and Credit Role Accreditation Council for Graduate Medical Education Review Committee for Surgery.
Q: What advances does your training method provide over existing approaches?
Moore: Our advanced colonoscopy training system utilizes a manikin embedded with sensors that allow us to identify, through automated performance feedback, a physician’s skill level for maneuvering the device and locating polyps. The manikin is adaptable for various patient types, which provides physicians with the opportunity to improve proficiency.
Q: How will your research improve patient health and experience?
Miller: Our training system will improve patient health by improving physicians’ ability to identify and locate polyps. This is vital because early detection is directly related to patient outcomes with colorectal cancer. Our system will also help reduce health care costs by providing a high level of efficient and effective training for medical residents without the need for expert oversight.
Q: This project includes collaboration with researchers from the College of Medicine. Could you tell us more about that collaboration?
Moore: This project utilizes an interdisciplinary research team to guide the design and deployment of our training system to improve the impact of the work. I bring expertise in tissue-to-instrument modeling and medical training device development, while Professor Miller is an expert in the design and evaluation of complex training systems, graphical user interfaces and simulation. Drs. Pauli and Haluck are practicing surgeons and professors in the College of Medicine. Their clinical expertise allows the accurate translation of fundamental research to the clinic.
Q: How do you see this improving the training process for residents? If you had access to this as a trainee, what would be different for you?
Pauli: Despite advancements in our understanding of how trainees learn complex procedures, the best methods for training someone in a psychomotor task — or a movement-based activity that requires integrated knowledge — remain unknown. Presently, residents learn through a mixture of simulated endoscopy procedures and by assisting or participating in colonoscopy procedures on real patients. But between these two methods of learning, there is a lot of room for improvement. For example, current colonoscopy simulators do not provide force feedback to trainees, who need to learn when they are applying excessive force to the colon wall. Excessive force can lead to a perforation in a live patient. Additionally, the simulated model in our study will utilize a real endoscope, enabling trainees hands-on experience with the very same device they will use clinically. We hope to utilize this training model to supplement how our trainees learn to perform safe and effective colonoscopy procedures.