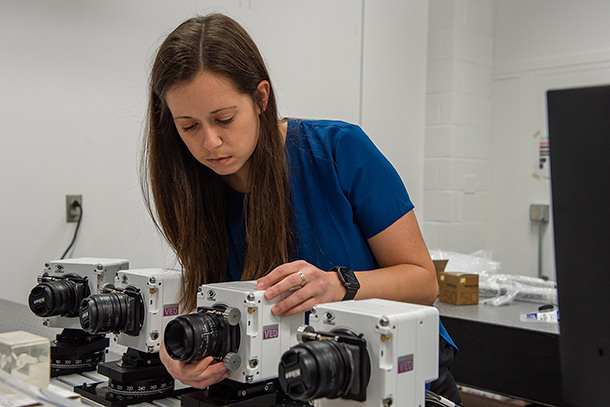
Melissa Brindise, Penn State assistant professor of mechanical engineering, adjusts a high-speed camera that she will use in particle image velocimetry, which tracks fluid flow speeds and dynamics in aneurysm models. Credit: Kelby Hochreither/Penn State
Career development award to assess risk factors of aneurysm rupture
May 31, 2022
By Mariah Chuprinski
UNIVERSITY PARK, Pa. — Brain aneurysms are dangerous — causing death or neurological deficits if they rupture. But over two-thirds of them are stable, according to a 2016 study. How do practitioners know when to operate and when to leave them alone?
The answer is complicated, according to Melissa Brindise, Penn State assistant professor of mechanical engineering. She recently received a three-year, $231,000 career development award from the American Heart Association to study factors that may increase the risk of an aneurysm rupture.
“When we study blood flow from an intracranial aneurysm, we typically only see it from one perspective, that is, when patients are lying down with a resting heart rate in an MRI machine,” Brindise said. “That single position makes MRI data insufficient, as we don’t know what the flow looks like when heart rate or blood pressure change, or when the patient moves around. We believe additional tools and different types of measurements can tell us more about aneurysms.”
Brain aneurysms occur when there is a bulge in a blood vessel, according to Brindise, usually at a location where three or more blood vessels converge. A rupture causes uncontrolled bleeding in the brain, which is closely followed by a stroke. Ruptures are fatal 45% of the time, according to Johns Hopkins Medicine, and survivors typically experience lasting neurological damage.
“Since they’re asymptomatic, aneurysms are really hard to discover,” Brindise said. “Usually, they are only identified if a patient happens to get a head CT scan for another reason. We do not yet know exactly why they form, but certain factors like genetics play a role."
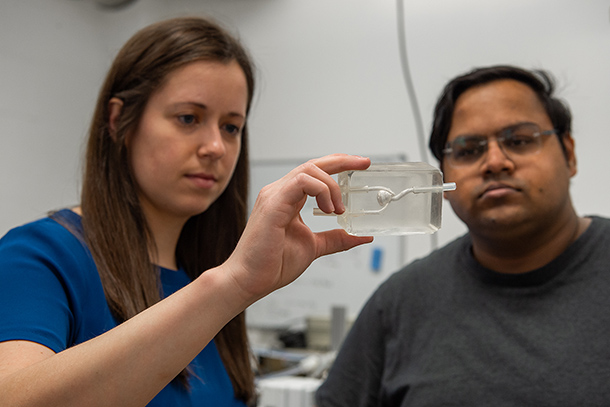
Brindise and Nikhil Shirdade, doctoral student in mechanical engineering, study a 3D model of an aneurysm bulge. Credit: Kelby Hochreither/Penn State. All Rights Reserved.
Brindise will use particle image velocimetry to track fluid flow speeds and dynamics in brain aneurysm models using high-speed laser lights and cameras. In PIV, luminous particles are placed in a blood-analog fluid, illuminated with a laser, and tracked over time to evaluate the fluid velocity and motion.
“We will make 3D-printed models of aneurysms, create an experimental flow loop, and then run the particles through the loop, mimicking what it would look like in a patient’s brain,” Brindise said. “This will determine what flow dynamics are occurring so that we can make predictions of how the aneurysm would likely develop over time if it was actually in someone’s brain.”
Using PIV, the researchers will measure three risk factors: wall shear stress, which quantifies the stress caused by blood on the walls of the blood vessel; oscillatory shear index, which measures the blood moving back and forth along the vessel wall; and resonance time, which measures how long blood sits near a vessel wall.
“Currently, the only way to assess whether an aneurysm will rupture is the shape and size of the aneurysm sac as it appears in clinical imaging, like an MRI or CT scan,” Brindise said. “Our idea that we are going to test is that transient elements — such as changing heart rate, the orientation of the patient, the inflow angle of the blood vessel and blood flow velocity — matter just as much as the shape of the aneurysm sac.”
The only way to check on blood flow in an aneurysm is through MRI imaging. Brindise wants that to change.
“MRI imaging is good, but not good enough,” Brindise said. “It doesn’t tell the whole story. Long term, we would like to build more advanced tools that can get a more complete picture of the aneurysm in order to make the best decision regarding the risk of rupture metrics.”
The study, Brindise hopes, will uncover preliminary data that can be a springboard for future projects. Long term, Brindise hopes her work can help physicians make decisions on treating aneurysms.
“The long-term goal is for doctors to use our physics-driven data analysis to make more accurate clinical decisions on whether to treat aneurysms,” Brindise said.
As part of the early career grant, Brindise will receive mentoring from three Penn State faculty members: Mary Frecker, professor and head of the Department of Mechanical Engineering, Patrick Drew, associate professor of neural engineering and neurosurgery, and Ephraim Church, assistant professor of neurosurgery, radiology and neurology at the Penn State College of Medicine.