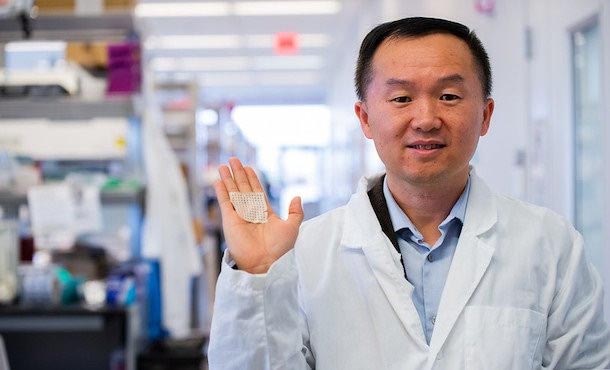
Jian Yang with a sample of his innovative wound dressing. IMAGE: TYLER HENDERSON
Academia-enterprise partnership aims to help people with diabetes
Innovative wound dressing would help reduce life-threatening infections, amputations for diabetic patients
2/4/2020
By Jamie Oberdick
UNIVERSITY PARK, Pa. — For a healthy person, a minor cut on the leg or foot is no big deal, something that only requires a bit of antiseptic and a small bandage. For a person with diabetes, it can become a much bigger problem.
“With patients with diabetes, small cuts and scratches may become a big deal as the wound may have issues with healing, and an infection can develop,” said Jian Yang, professor of biomedical engineering and Lloyd & Dorothy Foehr Huck Chair in Regenerative Engineering at Penn State. “Without proper medical care, such an infection can be life threatening and maybe even fatal. Even if no infection develops, cuts on the feet or legs can take a very long time to heal for a diabetic patient, greatly affecting walking and exercising and in turn, reducing quality of life.”
Most of the current wound-dressing products for diabetic patients are either not strong enough, lack long-term antimicrobial properties or do not have tissue adhesion properties, limiting their healing effectiveness. To solve this issue, Yang’s Transformative Biomaterials and Biotechnology Lab (TBBL) at Penn State is partnering with Xingguo Cheng, chief scientific officer with Dynamic Entropy Technology LLC (DET), a biomedical research company based in San Antonio, Texas to develop a strong, adhesive, antimicrobial wound dressing that is created by combining existing Penn State-developed technology and existing DET-developed technology.
Building a successful partnership
The road to this collaboration began in 2006, when Yang and Cheng met for the first time. Together, they talked informally about potential collaborative biomaterial projects. These talks ultimately culminated in the two researchers teaming up to apply for a Small Business Technology Transfer (STTR) grant from the National Institutes of Health (NIH) for development of an improved diabetic-wound dressing.
They ultimately submitted a Phase I proposal to the NIH’s National Institute of Diabetes and Digestive and Kidney Diseases. The STTR program is divided into three phases, and Phase I focuses on feasibility and proof of concept. The proposal was accepted and in September 2019, they received a STTR grant for $225,000.
The Penn State technology is a unique antibacterial and antifungal citrate adhesive material developed by TBBL that helps the dressing adhere on a wound to keep it covered for better healing. It also prevents infection by killing both bacteria and fungi that are normally found in slow-healing wounds or diabetic wounds. The DET-developed process enables the formation of a collagen-based biomaterial that can include non-collagen materials for structural strength via electrochemical deposition.
Combining the technologies allows an antibacterial and antifungal wound-dressing device with both robust mechanical strength and structures similar to the dense cutaneous tissue of the human foot, making it ideal for cutaneous wound healing.
“Our wound care product would be unique in terms of dual antibacterial and sustainable anti-fungal effects; dual degradation mechanism via an enzymatic process and hydrolysis; better reproducibility than biological allografts; suture-less wound closure due to strong tissue adhesion; and excellent biocompatibility,” Cheng said.
Solving the foot ulcer problem
This would be very beneficial for diabetes treatment, because foot ulcers are among the most common wounds suffered by diabetic patients. In the United States, the estimated number of people over 18 years of age with diagnosed and undiagnosed diabetes is 30.2 million individuals. Foot ulcers will develop in about one in four of these patients.
“The U.S. annual health care cost of just managing diabetic foot ulcers alone is estimated to be $9 billion to $13 billion,” Cheng said.
Foot ulcers are a serious problem for people with diabetes, Yang noted.
“Foot ulcers can ultimately lead to amputation,” Yang said. “About 230 amputations take place every day in the United States as a result of diabetes. These numbers speak to the significance. If successful, our proposed wound-dressing technology can help millions of patients in the United States and will generate a profound medical and societal impact.”
Cheng said that the product may also be useful for general skin-wound healing for cuts, surgery wounds, burns and other wounds.
Getting innovation to the people
Advancing biomedical technologies such as this wound dressing into the market and to health care providers for use on patients is always a significant challenge. Yang said that partnering with companies is an effective way to translate research into a usable product. The Penn State and DET team plans to use the Phase I STTR grant to first establish the feasibility of combining the two unique technologies for the development of the novel wound-dressing technology. After Phase I, the team will then seek NIH Phase II program support to further develop the technology and demonstrate the efficacy to treat diabetic wounds using a large animal model.
The objective of STTR program’s third and final phase is commercialization of a final product based on the Phase I and Phase II research and development activities. The STTR program does not provide funding for this, leaving it up to the small business to pursue financing goals on their own. Even with the project still at Phase I, DET is working on ideas to get their potential new wound dressing to market.
“While we are going through the phases of the grant, the DET team will develop and implement a commercialization plan that would lead to Federal Drug Administration approval and eventual entry to market,” Yang said.
The power of business-higher education partnerships
DET’s work on a commercialization plan for the wound dressing research is an example of why having strong relationships with businesses is important for university researchers, Yang said.
“Building a healthy and productive academia-enterprise partnership is key for technology translation and commercialization,” Yang said. “There have been so many new scientific discoveries or new technologies that have been developed but are mostly shown in publication forms. The return on investment often is poor due to relatively low efficiency for technology transfer from academia to industry. I believe that scientists, especially those who conduct translational research, should have a spirit of business in order to maximize the impact of their research.”
Yang himself has experience in the enterprise world. In 2015 he co-founded Aleo BME Inc., which is a Penn State spin-off company located in Innovation Park on the University Park campus. The company develops medical devices for wound healing and treatment and in January launched its first medical product, ElaSkinÒ Liquid Bandage, an FDA 510K cleared Class I medical device. It is the first peelable and skin-like elastic skin protectant ideal for the prevention and treatment of skin irritations, minor wounds, small cuts, heel blisters, skin cracks and scrapes.
In addition, Yang’s citrate biomaterial technologies have been licensed to a few other medical device companies, including Acuitive Technologies Inc. and Tara Biosystems Inc.
“We have noted a rapid increase in examples of scientists starting up small businesses or getting involved in technology translation activities by partnering with companies,” Yang said. “The NIH STTR program is facilitating such academia-enterprise collaborations for technology translation, including our current project with DET. Academic-enterprise collaboration is a complementary, win-win situation that will enable many biomedical innovations, like our diabetic wound dressing, to reach the marketplace and benefit public health.”