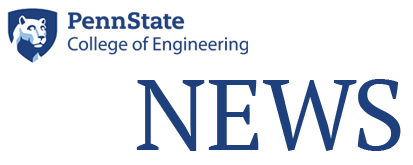
CT Scan showing the absence of blood flow to left brain. The patient has ischemic stroke or cerebrovascular disease. IMAGE: ISTOCK/@SITTITHAT TANGWITTHAYAPHUM
NIH grant recipients to study why some blood clots can't be cleared
6/29/2020
By Jamie Oberdick
UNIVERSITY PARK, Pa. — A team of Penn State and U.S. Food and Drug Administration researchers have received a four-year, $2.49 million grant from the National Institutes of Health to understand why certain blood clots that cause strokes cannot be removed.
“If we can understand more about these clots and the surrounding environment, we hope to then find ways to be able to safely remove them,” said Keefe B. Manning, associate dean of the Penn State Schreyer Honors College, professor of biomedical engineering and co-primary investigator of the study.
Strokes occur when the blood supply to the brain is interrupted or reduced. Two main types of strokes exist, hemorrhagic, caused by leaking or bursting blood vessels, and ischemic, caused by a blockage or narrowing in a blood vessel. A common type of blockage is a thromboembolism, a clot that is dislodged and moves downstream to another section of the circulatory system. In the United States, 700,000 acute ischemic strokes occur each year.
While stent retrievers, tiny, self-expanding stents used to remove blood clots in the brain, continue to improve for recanalization of blood clots — which is the reopening of a previously occluded passageway within a blood vessel — more than 15% of thromboemboli still cannot be cleared. In addition, another 17% of patients die within 90 days despite successful restoration of blood flow.
“Understanding the exact nature of the blood clots that are very hard to remove is a challenge since we cannot get to them,” Manning said. “We are relying on a lot of peripheral data — from patient imaging to the patient’s blood biochemistry to testing patient clots that have been removed — to understand material properties and histology from that perspective.”
To solve this problem, Manning and fellow researchers propose a better understanding via computer modeling of the entire progression of AIS, from clot formation to removal. To achieve this, they will develop computational models that simulate the clot formation, the detachment of the clot from its original location, lodging and adhesion in the cerebral vasculature, and clot removal via applied forces from a thrombectomy device such as a stent retriever.
This mimics how computer models are used to forecast weather and design rockets and aircraft, according to Francesco Costanzo, co-PI on the grant and associate head of engineering science and mechanics and professor of engineering science and mechanics, mathematics, mechanical engineering and biomedical engineering.
“There is now a great deal of the design of the performance of an aircraft that can be done on a computer rather than in the shop,” Costanzo said. “We are striving to achieve the same goal in medicine. We would like to be able to monitor the health of a patient, predict when something might go wrong and prepare for optimal interventions when some problem does indeed occur. All of this effort requires the acquisition and processing of an enormous amount of information, and computational technology is a key factor in achieving our goal.”
The researchers will validate the models with ex vivo mock circulatory flow loops that enable real-time tracking of clot growth and embolization, which is the passage and lodging of the clot within the bloodstream. The mock circulatory flow loops will also enable AIS blockage to be simulated in physiologically accurate scenarios. Other considerations in the models include patient-specific anatomy and blood chemistry.
Armed with the modeling and additional data, the researchers aim to provide a deeper understanding of AIS formation that would not only lead to better outcomes for stroke victims, but for other types of patients as well.
“We may be able to apply any technology that is developed from the grant to other blood clots that get stuck in other areas,” said Manning.
The research is an example of beneficial collaboration within the Penn State system, according to Scott Simon, associate professor of neurosurgery at the Milton S. Hershey Medical Center and co-PI of the study.
“With regard to designing better stroke devices, we do not have the computational expertise or resources here in Hershey and the University Park campus doesn’t have the clinical expertise or the patients to effectively impact this disease process,” Simon said. “Together we can bring impressive reservoirs of knowledge and skills from many perspectives to solve pressing clinical problems.”
Along with Costanzo, Manning and Simon, Brent Craven, staff fellow with the U.S. Food and Drug Administration, also serves as co-PI on the grant.